Obesity
- Modest weight loss of 5–10% of starting weight can lead to significant health benefits.
- Substantial weight loss offers even greater improvements in obesity-related comorbidities.
Health risks associated with overweight and obesity in adults
| Body system | Health risk |
|---|---|
| Cardiovascular | Stroke Coronary heart disease Cardiac failure Hypertension |
| Endocrine | Type 2 diabetes Polycystic ovary syndrome |
| Gastrointestinal | Non-alcoholic fatty liver disease Gallbladder disease Pancreatic disease Gastro-oesophageal reflux disease Cancers of the bowel, oesophagus, gall bladder and pancreas |
| Genitourinary | Chronic kidney disease – glomerulopathy End-stage renal disease Kidney cancer Kidney stones Prostate cancer Stress urinary incontinence (women) Sexual dysfunction (men) |
| Pulmonary | Obstructive sleep apnoea Obesity hypoventilation syndrome Asthma |
| Musculoskeletal | Osteoarthritis – especially the knees Spinal disc disorders Lower back pain Disorders of soft tissue structures such as tendons, fascia and cartilage Foot pain Mobility disability (particularly in older adults) |
| Reproductive health | Menstrual disorders Miscarriage and poor pregnancy outcome Infertility/sub-fertility Breast cancer (postmenopausal women) Endometrial cancer Ovarian cancer |
| Mental health | Depression Eating disorders – binge eating disorder Reduced health – related quality of life |
| Adapted with permission from National Health and Medical Research Council. Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. Canberra: NHMRC, 2013 | |
Weight management in general practice
General practitioners are often the first healthcare providers to identify overweight or obesity. Treatment should be individualised with careful consideration given to the severity of the problem and associated complications using the 5As approach for weight management: Ask and Assess, Advise, Assist and Arrange
| Establish a therapeutic relationship, communicate and provide care in a way that is person centred, culturally sensitive, non-directive and non-judgemental | |||||
| Ask and Assess | Standard care | Active management | |||
|---|---|---|---|---|---|
| BMI <25 | BMI 25–29.9 | BMI 30–34.9 | BMI 35–39.9 | BMI >40 | |
| Routinely assess and monitor BMI and waist circumference (WC) | Routinely assess and monitor BMI and WC Discuss if BMI and/or WC increasing Screen for and manage comorbidities | Routinely assess and monitor BMI and WC Discuss health issues Screen for and manage comorbidities Assess other factors related to health risk – Blood pressure – lipid profile – fasting glucose – liver function tests Ask about symptoms of sleep apnoea and depression | |||
| Advise | Promote benefits of healthy lifestyle Explain benefits of prevention of weight gain and maintenance of healthy weight | Promote benefits of healthy lifestyle Explain benefits of weight management | |||
| Assist | Assist in setting up weight loss program: Advise lifestyle interventions Based on comorbidities, risk factors and weight history, consider adding intensive weight loss interventions (eg. VLEDs, pharmacotherapy, bariatric surgery) Tailor the approach to the individual Refer to multidisciplinary team for specialist treatment recommendations. Suitable patients include : – BMI >40 – BMI >35 with any serious comorbidity – BMI 30–35 with serious comorbidity and a positive weight trajectory | ||||
| Arrange | Review and monitoring Long term weight management Referral to specialist weight management clinic if indicated | ||||
| BMI (kg/m2) | Classification | Men WC 94–102 cm Women WC 80–88 cm | Men WC >102 cm Women WC >88 cm |
|---|---|---|---|
| 18.5–24.9 | Normal weight† | – | – |
| 25–29.9 | Overweight | Increased | High |
| 30–34.9 | Obese class I | High | Very high |
| 35–39.9 | Obese class II | Very high | Very high |
| ≥40.0 | Obese class III | Extremely high | Extremely high |
| * Disease risk for type 2 diabetes, hypertension and cardiovascular disease † Increased WC can also be a marker for increased risk even in persons of normal weight Reproduced from the Scottish Intercollegiate Guidelines Network (SIGN). Management of obesity. A national clinical guideline. Edinburgh: SIGN; Year. (SIGN publication no. 115). [cited 10 July 2013]. Available from URL: www.sign.ac.uk | |||
- Lifestyle Interventions as First-Line Treatment
- Despite difficulties, lifestyle interventions remain the first-line treatment for overweight and obesity.
- Initial approach should focus on healthy eating, reducing energy intake, increasing physical activity, and reducing sedentary behavior, following Australian Dietary Guidelines 2013.
- Psychological therapies can support behavior change and may be beneficial.
- Healthy Eating:
- Emphasize adherence to Australian Dietary Guidelines 2013.
- Focus on balanced meals with appropriate portion sizes.
- Encourage consumption of fruits, vegetables, lean proteins, and whole grains.
- Limit intake of processed foods, sugary beverages, and high-calorie snacks.
- Exercise Guidelines
- Duration: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, spread over several days.
- Intensity: Exercise should be of moderate intensity, where breathing and heart rate increase but conversation is still possible.
- Types of Exercise: Incorporate a combination of aerobic exercise (e.g., brisk walking, cycling) and strength training (e.g., weightlifting, bodyweight exercises).
- Flexibility and Balance: Include flexibility and balance exercises to improve overall fitness and reduce risk of injury.
- Gradual Progression: Start with manageable exercise levels and gradually increase duration and intensity as fitness improves.
- Avoidance of Certain Fats
- Saturated Fats: Limit intake of saturated fats found in fatty meats, butter, cheese, and processed foods.
- Trans Fats: Avoid trans fats found in fried foods, baked goods, and processed snacks.
- Focus on Healthy Fats: Include sources of healthy fats such as avocados, nuts, seeds, and oily fish like salmon and mackerel.
- Behavioral Strategies
- Goal Setting: Help patients set realistic, achievable goals for weight loss and lifestyle changes.
- Self-Monitoring: Encourage keeping food and activity journals to track progress and identify areas for improvement.
- Problem Solving: Teach problem-solving skills to overcome barriers to healthy eating and exercise.
- Social Support: Encourage involvement in social support networks, such as group exercise classes or weight loss support groups.
- Long-Term Maintenance
- Emphasize sustainability: Encourage lifestyle changes that can be maintained in the long term.
- Regular Monitoring: Schedule regular follow-up appointments to monitor progress and provide ongoing support.
- Adaptation: Help patients adapt to setbacks and challenges by providing ongoing encouragement and guidance.
Intensive interventions
- very low energy diets (VLEDs)
- pharmacotherapy
- bariatric surgery
Average weight loss of subjects completing a minimum 1 year weight management intervention; based on review of 80 studies (N=26 455; 18 199 completers [69%])

Very Low Energy Diets (VLEDs)
- Indications
- Recommended for patients with a BMI >30 or BMI >27 with obesity-related comorbidities.
- Effectiveness
- Under medical supervision, VLEDs can induce rapid weight loss, achieving an average of 18–20% reduction.
- Rapid weight loss improves glycaemic control, blood pressure, and reduces total cholesterol.
- Mechanism
- Involves replacing all meals with a specific meal replacement formula during the intensive phase.
- High protein-low carbohydrate diets induce fat burning and mild ketosis, suppressing hunger and promoting satiety.
- Duration and Safety
- Treatment duration is typically 8–12 weeks, but safe year-long use under strict medical supervision is possible.
- VLEDs are safe and effective for long-term weight maintenance, either intermittently or on-demand.
- Considerations
- Not suitable for all obese patients; costs associated with meal replacements should be considered.
- Contraindications include pregnancy, lactation, children, adolescents, elderly, psychological disturbances, alcohol or drug abuse, porphyria, recent myocardial infarction, or unstable angina.
- Monitoring and Support
- Monitoring and support are crucial for success.
- Training on the use of VLEDs should be sought by practices intending to use this intervention effectively with suitable patients.
Pharmacotherapy
Pharmacotherapy should complement, not replace, lifestyle interventions, similar to management strategies for hypertension, diabetes, and cardiovascular disease.
Drug therapies modify energy regulation by reducing appetite, increasing satiety with smaller meals, and prolonging satiety after meals.
Weight-loss pharmacotherapy should be considered for:
- Patients with BMI >30 kg/m².
- Patients with BMI 27–30 kg/m² with obesity-related complications.
- Lower BMI thresholds may apply to Aboriginal and Torres Strait Islander and Asian populations.
Phentermine
- Phentermine is a sympathomimetic agent that suppresses appetite.
- Effectiveness
- Studies show an average weight loss of 3.6 kg over six months compared to placebo, with a noted increase to 4.5 kg using 15 mg of phentermine.
- Dosage and Administration
- Available as a slow-release resin in doses of 15, 30, and 40 mg.
- Administered once daily in the morning, starting at 15 mg and adjusting as needed to minimize side effects.
- Common Side Effects
- Typically mild but include dry mouth, insomnia, agitation, constipation, and tachycardia.
- Contraindications
- Not suitable for patients with
- cardiovascular disease
- anxiety disorders
- hyperthyroidism
- history of drug or alcohol abuse
- concurrent use of monoamine oxidase inhibitors
- pregnant or breastfeeding.
- Not suitable for patients with
- Usage Cautions
- Use cautiously in patients with hypertension, cardiac arrhythmias, or seizures.
- Regular monitoring of blood pressure is recommended.
- Historical and Current Usage
- Historically used as a short-term medication in the US and Australia, but now approved for long-term use when combined with topiramate.
- Safety and Monitoring
- Low addiction potential and minimal evidence of serious side effects in long-term monotherapy.
- Recommended monitoring includes initial evaluation, reassessment at three months, then regularly (monthly during dose escalation and at least every three months thereafter).
- Criteria for Long-Term Prescription
- Appropriate for patients with low to intermediate cardiovascular risk and no serious cardiovascular conditions.
- Patients should not have serious psychiatric conditions or a history of substance abuse.
- No significant increase in pulse or blood pressure during treatment.
- Follow a specific efficacy-safety stopping rule.
Orlistat
- Mechanism of Action
- Orlistat inhibits pancreatic and gastric lipases, reducing absorption of dietary fat.
- Unique Weight Loss Approach
- It’s the only approved weight-loss medication that primarily works by inhibiting fat absorption, rather than suppressing appetite.
- Dosage and Fat Excretion
- Administered at 120 mg three times daily with meals, leading to approximately 30% of oral fat excretion in stools.
- Weight Loss and Safety
- A mean weight loss of 2.9–3.4% is observed after one year of Orlistat use, with a relatively good long-term safety record.
- Side Effects
- Side effects stem from fat malabsorption and include steatorrhoea, oily spotting, flatulence, faecal incontinence, fat-soluble vitamin deficiencies, and calcium oxalate kidney stones.
- Management of Side Effects
- Gastrointestinal side effects, the primary reason for therapy discontinuation, can be mitigated by adhering to a low-fat diet and increasing dietary fibre.
- Effect on T2DM
- Orlistat has shown improvements in glycated haemoglobin (HbA1c) by 0.4% in individuals with T2DM compared to controls.
- Prevention of T2DM
- The XENical in the prevention of Diabetes in Obese Subjects (XENDOS) study found a 37% reduction in T2DM incidence over four years with Orlistat when added to lifestyle therapy for obese patients.
Liraglutide
- Mechanism of Action
- Liraglutide is a glucagon-like peptide-1 (GLP-1) agonist primarily used to treat T2DM, controlling hyperglycaemia without causing hypoglycaemia or weight gain.
- Weight Management
- Its side effect profile, including decreased appetite and subsequent weight loss, has led to its approval as a weight management drug.
- Clinical Efficacy
- Large-scale studies have shown that liraglutide 3 mg leads to significant weight loss (5.6 kg or 5.4%) compared to placebo after one year, with improvements in cardiometabolic risk factors.
- Administration and Dosage
- Liraglutide can be administered independently of meals as a subcutaneous injection into the abdomen, thigh, or upper arms.
- The starting dose is 0.6 mg once daily, which can be increased to 3 mg with gradual increments of 0.6 mg over at least one week to improve gastrointestinal tolerability.
- Side Effects
- Common gastrointestinal side effects include nausea, vomiting, diarrhoea, constipation, and dyspepsia, which can be mitigated by gradual dose escalation.
- Most gastrointestinal symptoms are mild to moderate, transient, and diminish within days or weeks with continued treatment.
- Liraglutide-induced weight loss is associated with an increased incidence of symptomatic gallstones and, rarely, pancreatitis.
- Contraindications
- Liraglutide should not be used in individuals with severe renal or hepatic insufficiency, pregnancy, past history of pancreatitis, major depression, or psychiatric disorders.
- Cardiovascular Safety
- Liraglutide appears to have a strong evidence base for cardiovascular safety, especially in those at high cardiovascular risk or with glucose intolerance such as T2DM or pre-diabetes.
- Drawbacks
- Drawbacks include high costs (approximately $380/month in Australia) and gastrointestinal side effects that may limit its use.
Off-label pharmacotherapy
- Topiramate for Obesity
- Topiramate, an anticonvulsant, is used off-label for obesity due to its weight loss side effect.
- Effective doses range between 25 and 100 mg daily, with an expected weight loss of 3.4–5.0 kg.
- Common side effects include paraesthesia, dry mouth, constipation, altered taste sensation, insomnia, and dizziness.
- Serious side effects include closed-angle glaucoma and increased suicidal thoughts.
- Contraindications include pregnancy, history of glaucoma, or renal stones.
- Phentermine/Topiramate Combination
- This combination is approved in the US for obesity treatment.
- Studies show weight reduction of 5.1–10.5% and improvement in metabolic parameters.
- Some patients cannot tolerate the combination due to topiramate side effects.
- Other Medications
- Naltrexone/bupropion combination and lorcaserin are approved in the US but not in Australia.
- The combination provides average weight loss of 4.8%.
- Lorcaserin suppresses appetite with an expected weight loss of 3.6%.
- Common side effects include nausea, vomiting, headache, dizziness, and dry mouth.
Monitoring and Stopping Rules
- Patients should be closely monitored for the first three to four months to assess safety, tolerability, and efficacy.
- Immediate discontinuation is necessary for safety or significant tolerability issues.
- If insufficient weight loss (<5%) is observed at three to four months, discontinuation is recommended due to likely outweighed long-term benefits by risks and costs.
Pharmacotherapy for Obesity and T2DM
- Management of obesity is beneficial for treating T2DM.
- First-line therapy for T2DM is metformin, with consideration of weight profile of second-line medications.
- Recent cardiovascular outcome trials show positive data for antidiabetic agents like empagliflozin and liraglutide.
Long-Term Use of Pharmacotherapy
- Despite efficacy, discontinuation of weight loss drugs is common due to concerns about side effects, costs, and perceived unnecessary use.
- However, if well tolerated and effective, pharmacotherapy should be continued for long-term weight maintenance and to limit weight regain.
- Current medications show no significant long-term safety concerns, but ongoing large cardiovascular outcome studies are being conducted.
Surgery – bariatric
- Criteria for Surgery
- BMI >40 kg/m2.
- BMI >35 kg/m2 with one or more obesity-related complications.
- Endorsement by Diabetes Organizations
- Bariatric-metabolic surgery proposed as a treatment option for T2DM.
- Recommended for:
- Individuals with T2DM and BMI ≥40 kg/m2.
- Individuals with BMI 35–40 kg/m2 with inadequate glycaemic control despite lifestyle and optimal medical therapy.
- Absolute Contraindications
- Few absolute contraindications include
- contraindications to general anesthesia
- serious blood or autoimmune disorders
- active substance abuse
- severe untreated psychiatric illness
- limited life expectancy due to organ failure or malignancy
- Few absolute contraindications include
- Suitable for younger patients at risk of obesity-related complications but caution advised for older patients (>65 years) due to increased postoperative risks.
- Pregnancy Considerations
- Associated with reduced risks of gestational diabetes but increased risks of pre-term birth and small-for-gestational-age infants.
- Women of childbearing potential should avoid pregnancy pre-operatively and 12–18 months postoperatively.
- Close monitoring and nutritional supplementation are essential for pregnant patients post-surgery.
- Patient Commitment
- Patients must be willing and motivated to adhere to postoperative lifestyle changes, nutritional supplementation, and follow-ups for safety and success
Pre-operative optimisation of obesity-related complications
| Obesity-related complication | Pre-operative screening and optimisation | Improvement after weight loss post-surgery |
|---|---|---|
| Type 2 diabetes mellitus | Glycated haemoglobin (HbA1c) and fasting glucose to screen for diabetesAim for good glycaemic control (HbA1c <7%) prior to surgery | Better glycaemic control and a reduced medication burdenDiabetes remission in some cases |
| Cardiovascular disease | Electrocardiogram (ECG) and cardiac risk assessmentReferral to cardiology if high cardiovascular risk, presence of cardiac symptoms or abnormal ECG | Reduction of cardiovascular morbidity of >50% (compared to body mass index [BMI] and age matched controls) |
| Non-alcoholic fatty liver disease | Liver function testsConsider abdominal ultrasound scan if liver function test increased, specifically to detect fibrotic liver disease | Improved liver histological appearancePotential regression of established liver disease |
| Obstructive sleep apnoea (OSA) and asthma | Screening questionnaire (eg STOP-BANG) to identify those at risk for OSARefer to sleep specialist if STOP-BANG score ≥327 | Significant improvement in apnoea–hypopnoea indexRemission of OSA in some cases |
Types of Bariatric Surgery
- Gastric Bypass (Roux-en-Y)
- Involves creating a small pouch from the stomach and connecting it directly to the small intestine.
- Restricts food intake and reduces absorption of nutrients.
- Sleeve Gastrectomy
- Involves removing a large portion of the stomach, leaving a smaller sleeve-shaped stomach.
- Restricts food intake and reduces hunger-inducing hormones.
- Gastric Banding
- Involves placing an adjustable band around the upper part of the stomach to create a small pouch.
- Limits food intake by creating a feeling of fullness.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
- Involves removing a portion of the stomach and rerouting the small intestine to limit absorption.
- Most complex and effective in terms of weight loss but carries higher risks.
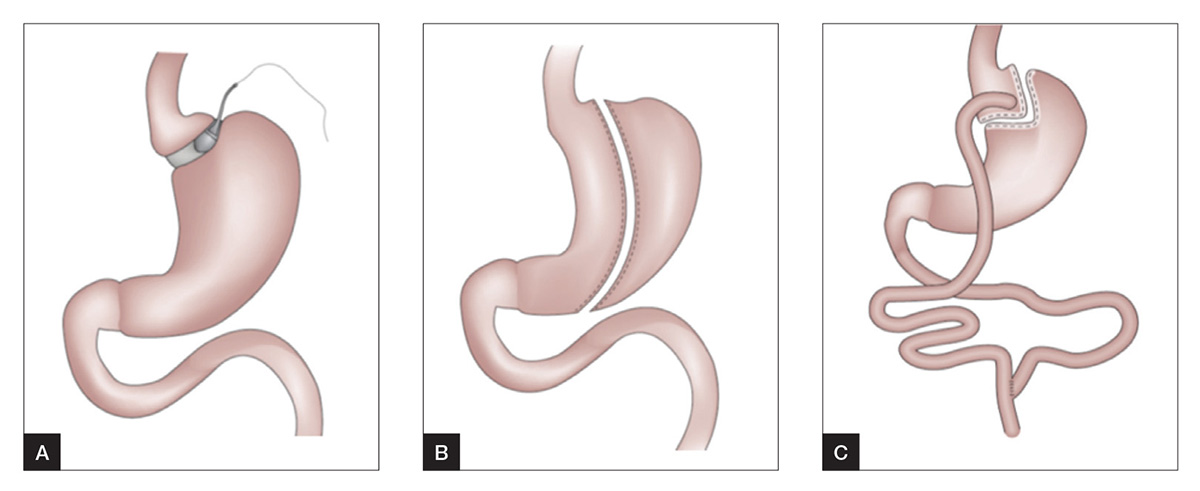
A. Adjustable gastric band = B. Sleeve gastrectomy = C. Roux-en-Y gastric bypass
Complications of Bariatric Surgery
- Immediate Complications
- Infection
- Bleeding
- Blood clots
- Anesthesia-related complications
- Short-term Complications
- Dumping syndrome (nausea, vomiting, diarrhea)
- Nutrient deficiencies (vitamin and mineral deficiencies)
- Dehydration
- Gallstones
- Long-term Complications
- Weight regain
- Malnutrition
- Gastrointestinal issues (ulcers, strictures)
- Hernias
- Psychological issues (depression, body image concerns)
| Adverse events | Presentation | Management |
|---|---|---|
| Acute complications | ||
| Surgical complications (eg leaks, perforations, obstruction, infection, haemorrhage) | Abdominal pain, tachycardia, breathlessness, drop in haemoglobin | Usually detected during immediate postoperative period and managed by the surgical team Presence of these symptoms should prompt urgent referral back to the surgical team |
| Hypoglycaemia (usually in patients with pre-existing diabetes) | Sweating, dizziness, headaches, palpitationsLow capillary blood glucose on testing | Fairly common, especially in patients on insulin or insulin secretagogues Stop sulphonylureas, and stop insulin or decrease doseClose self-monitoring of capillary blood glucose |
| Dumping syndrome | Abdominal pain, diarrhoea, nausea, flushing, palpitations, sweating, agitation, and syncope after meals rich in simple carbohydrates | Dietary modification, with small regular meals containing protein and complex carbohydrates Acarbose may be helpful in some refractory cases |
| Long-term complications | ||
| Iron-deficiency anaemia | Microcytic, hypochromic anaemia, lethargy, anorexia, pallor, hair loss, muscle fatigue | Oral iron supplements, consider intravenous iron for severe deficiency Vitamin C to increase iron absorptionRule out bleeding ulcers, neoplastic disease or diverticular disease |
| B12 deficiency | Macrocytic anaemia, leukopenia, glossitis, thrombocytopenia, peripheral neuropathy | Vitamin B12 repletion (oral or intramuscular) Prevention – B12 containing multivitamin supplementation Annual serum B12 level evaluation |
| Thiamine deficiency | Neurological symptoms, Wernicke’s encephalopathy in severe cases | Appropriate postoperative diet, with regular dietitian follow-up Screen for other nutritional deficiencies Thiamine supplementation |
| Over-restricted gastric band (for patients with adjustable gastric band) | Maladaptive eating, gastro-oesophageal reflux disorder, vomiting, regurgitation, chronic cough, or recurrent aspiration pneumonia | Reduce amount of fluid in gastric band Consider referral to bariatric surgeon for assessment of band position and function |
| Weight regain | Maximal weight loss usually achieved at one to two years after surgery, with some weight regain thereafter | For patients with laparoscopic adjustable gastric band – evaluation of band, adjust as required Consider adjuncts (eg very low energy diet, pharmacotherapy) Consider referral back to weight management clinic |
Monitoring Complications in General Practice
- Regular Follow-up
- Schedule regular follow-up appointments post-surgery to monitor progress and identify complications early.
- Medication review –
- Avoid nonsteroidal anti-inflammatory drugs (https://doi.org/10.1016/j.soard.2022.03.019)
- prevalence of peptic ulcers was 1.8% in this cohort of 41,380 patients
- Continuous NSAID-use (>30 days) is a significant risk factor for peptic ulcers after RYGB
- No increased risk was observed for temporary NSAID-use (<30 days)
- Adjust antihypertensives, lipid medications as appropriate. These medications should not be discontinued empirically
- Adjust diabetes medications. Requirement for anti-diabetes medications often decreases, and in many cases, diabetes remission is achieved. Preference for use of agents with favourable weight profile
- Medications with a narrow therapeutic index (eg warfarin, digoxin, lithium, antiepileptic medications) also require close monitoring and titration because of altered oral drug bioavailability following bariatric–metabolic surgery.
- Avoid nonsteroidal anti-inflammatory drugs (https://doi.org/10.1016/j.soard.2022.03.019)
- Nutritional supplements:
- Adult multivitamin and multimineral – containing iron, folic acid, thiamine, vitamin B12. Doses: two daily for sleeve gastrectomy or Roux-en-Y gastric bypass; one daily for adjustable gastric band
- Citrated calcium – elemental calcium 1200–1500 mg/day
- Vitamin D – titrate to 25-OH vitamin D levels >30 ng/mL. Typical dose required 3000 IU/day
- Additional iron and vitamin B12 supplementation as required, based on lab results
- Laboratory assessment:
- Full blood count, urea and electrolytes, liver function tests, uric acid, glucose, lipids (every 6–12 months)
- 25-OH vitamin D, iPTH, calcium, albumin, phosphate, B12, folate, iron studies (annually, more frequently if deficiencies identified)
- Gastrointestinal Symptoms
- Monitor for symptoms such as abdominal pain, nausea, vomiting, or changes in bowel habits, which could indicate complications like ulcers or strictures.
- Weight Management
- Monitor weight loss progress and watch for signs of weight regain, which may require additional intervention or support.
- Psychological Support
- Assess for psychological issues such as depression or body image concerns and provide appropriate support or referral to mental health professionals if needed.
- Screening for Long-term Complications
- Consider screening for long-term complications such as hernias or gallstones through physical examination or imaging studies if symptoms arise.