Urinary Tract Infections (UTI) kids
from RCH and eTG
- Signs and symptoms of UTI can be non-specific, and overlap with common viral illnesses, especially in younger children
- A urine sample is required to diagnose or exclude UTI where clinically suspected
- Consider UTI if fever without focus persists after 48 hours in young children
- it is difficult to distinguish pyelonephritis from cystitis, particularly in infants.
- If the child has bacteriuria and localising symptoms (such as dysuria, frequency, urgency or lower abdominal discomfort), and does not have fever (38°C or higher) or loin pain or tenderness, treat as acute cystitis.
- If the child has bacteriuria and either fever (38°C or higher) or loin pain or tenderness, treat as acute pyelonephritis.
Epidemiology
- Incidence child hood is 8%
- 5% children with fever will have UTI
- Boys disease of infancy (<1yr)
- More common in boys than girls during first year of life
- Girls peak incidence 6-12 months
History
- Infants and pre-verbal children often present with non-specific symptoms such as fever, vomiting, poor feeding, lethargy and irritability
- Older children may present with more typical symptoms such as dysuria, urinary frequency, lower abdominal and loin pain
- Ask about previous UTI
Examination
- Examination may be normal in UTI other than the presence of fever
- Lower abdominal or loin tenderness may be present
- Non-specific findings include dehydration and lethargy
Assessment of severity
- Clinical distinction between lower and upper UTI can be difficult, especially in younger children
- Cystitis is suggested by features such as dysuria, frequency, urgency and lower abdominal discomfort
- Pyelonephritis is suggested by systemic features such as fever, malaise, vomiting and loin tenderness
- Non-severe
- if the child does not have systemic features (eg tachycardia, nausea, vomiting), or sepsis or septic shock
- Severe
- if the child has systemic symptoms (eg tachycardia, nausea, vomiting), or sepsis or septic shock
- Non-severe
Investigation
Children with suspected UTI should have a urine sample collected; dipstick and microscopy screening can guide initial management. Check culture results after 24 hours to confirm or adjust management as appropriate
Urine samples should be collected prior to starting antibiotics (unless the child is seriously unwell and requires immediate IV therapy)
- Older children able to void on request can provide a midstream urine sample
- For younger pre-continent children, a clean catch is often suitable. Catheter or SPA may be required for seriously unwell infants
Urine Collection
- The perineal/genital area should be cleaned with saline-soaked gauze for 10 seconds before collecting midstream or clean catch urine
- Midstream urine (MSU): preferred method for toilet-trained children who can void on request — contamination rate 25%
- Clean catch: appropriate for pre-continent children who cannot void on request, but are not seriously unwell (yield may be improved by gently rubbing child’s suprapubic area with gauze soaked in cold fluid, see urine tests) — contamination rate 25%
- Suprapubic aspirate: gold standard — contamination rate 1%
- In/out catheter: useful if there is little urine in the bladder, such as after failed clean catch or SPA (discard first few drops of urine if possible to reduce contamination) — contamination rate 10%
- Bag urine: not recommended for culture due to high false positive rates — contamination rate 50%
Urine dipstick
- Urine dipstick is a useful screening test to guide initial management
- Positives suggestive of a UTI readings for
- nitrite (75% UTI probability)
- leukocyte esterase (30% UTI probability)
- Dipstick results are less reliable in neonates and young infants, particularly due to false negatives
Urine Microscopy and Culture
- Laboratory microscopy can complement dipstick results to guide initial management
- Bacteria and leucocytes on microscopy are suggestive of UTI. See notes section below
- Epithelial cells (squames) suggest skin contamination and a poorly collected sample. Consider recollection
- A positive culture with sufficient growth and pyuria confirms UTI
- Growth of a single organism at >108 CFU/litre (>105 CFU/mL) from any collection method suggests infection
- Growth of a single organism at lower counts of 106-8 CFU/litre (>103-5 CFU/mL) from catheter or SPA urine suggests infection, and from clean catch or MSU may indicate early infection
- Growth of any amount from SPA suggests infection
Other investigations
- Check renal function and consider renal ultrasound if the child is seriously unwell, or not responding to appropriate therapy after 48hrs
- Consider blood culture and lumbar puncture for unwell infants less than 4 weeks old, or if sepsis or meningitis is suspected at any age
Acute treatment pathogens
- E.Coli = 85%
- Proteus sp 6% (male organism)
- Klebsiella 5%
- E.faecalis 4% (<3month organism)
Treatment
- Oral antibiotics are usually appropriate
- Any child who is seriously unwell, and most infants under 3 months, should be admitted for initial IV antibiotics
- 3–7 day course for children with cystitis
- 7–10 day course for children with pyelonephritis
- Oral treatment
- For cystitis :
- Empirical Therapy for Acute Cystitis in Children
- First-Line Empirical Therapy (awaiting culture and susceptibility results):
- Trimethoprim + Sulfamethoxazole:
- Dosage: 4+20 mg/kg up to 160+800 mg orally, 12-hourly for 3 days.
- Suitable for children 1 month or older.
- Note 1: If a suitable trimethoprim formulation is available, consider using trimethoprim alone.
- Trimethoprim:
- Dosage: 4 mg/kg up to 150 mg orally, 12-hourly for 3 days.
- Note 2: Use only if a suitable formulation is available.
- Cefalexin:
- Dosage: 12.5 mg/kg up to 500 mg orally, 6-hourly for 3 days.
- Trimethoprim + Sulfamethoxazole:
- Modification Based on Culture and Susceptibility Testing:
- If the pathogen is resistant to empirical therapy but symptoms are improving:
- Do not modify therapy.
- If the pathogen is resistant and symptoms are not improving, switch to the narrowest spectrum antibiotic to which the pathogen is susceptible:
- Amoxicillin:
- Dosage: 15 mg/kg up to 500 mg orally, 8-hourly for 3 days.
- Amoxicillin + Clavulanate:
- Infant younger than 2 months: 15+3.75 mg/kg orally, 8-hourly for 3 days.
- Child 2 months or older: 22.5+3.2 mg/kg up to 875+125 mg orally, 12-hourly for 3 days.
- If the pathogen is resistant to empirical therapy but symptoms are improving:
- Alternatives for Resistant Pathogens:
- Norfloxacin:
- Dosage: 10 mg/kg up to 400 mg orally, 12-hourly for 3 days.
- Note 3 & 4: Use only if the pathogen is susceptible and other first-line options are unsuitable.
- Ciprofloxacin:
- Dosage: 12.5 mg/kg up to 500 mg orally, 12-hourly for 3 days.
- Note 5 & 6: Use only if the pathogen is susceptible and other first-line options are unsuitable.
- Norfloxacin:
- First-Line Empirical Therapy (awaiting culture and susceptibility results):
- Empirical Therapy for Acute Cystitis in Children
- For Non-severe pyelonephritis:
- Trimethoprim+sulfamethoxazole (child 1 month or older) 4+20 mg/kg up to 160+800 mg orally, Q12h 10 days. – OR –
- Trimethoprim 4 mg/kg up to 150 mg orally, Q12h for 10 days. – OR –
- Cefalexin 12.5 mg/kg up to 500 mg orally, Q6hfor 10 days. If clinical response is rapid, stop therapy after 7 days – OR
- Amoxicillin+clavulanate orally, for 10 days
- infant <2 months: 15+3.75 mg/kg, Q8h
- child >2 months: 22.5+3.2 mg/kg up to 875+125 mg, Q12h
- For cystitis :
- IV treatment – for SEVERE Pyelonephritis
- Do not delay antibiotic therapy for a child who is seriously unwell, even if a urine sample has not been obtained
- Recommended empiric IV antibiotics:
- (Gentamicin) + (Amoxicillin 50 mg/kg up to 2g Q6h – OR – ampicillin 50 mg/kg up to 2g Q6h)
- if Gentamycin is Contraindicated
- cefotaxime 50 mg/kg up to 1g, 8-hourly – OR –
- Ceftriaxone (child 1 month or older) 50 mg/kg up to 1g daily.
- Switch to oral antibiotics when clinically improved and/or as soon as tolerating oral antibiotics
| eTG listed | Antibiotics | Therapeutic dose | Prophylactic dose | Adverse effects | Targets | Notes |
|---|---|---|---|---|---|---|
| 1. | Trimethoprim (TMP) ‘Alprim’ | 4 mg/kg BD Max: 150 mg BD | 4 mg/kg Nocte Max: 150 mg Nocte | Nausea and vomiting Pruritus Rash, Stevens-Johnson syndrome Hyperkalaemia Thrombocytopenia Leucopenia | Escherichia coli Enterobacter spp. Klebsiella spp. Proteus mirabilis Coagulase (–) Staphylococcus aureus | Contraindicated in renal impairment and folate deficiency Multiple drug interactions Not recommended for children younger than 1 month |
| Trimethoprim–sulfamethoxazole (TMP–SMX) ‘Bactrim’ | 4 + 20 mg/kg BD Max: 16 0+ 180mg BD | 2 + 10mg/kg Nocte Max: 80 + 400mg Nocte | Same as TMP Hepatotoxicity Seizures, vertigo Peripheral neuropathy Kernicterus | Same as TMP Broader coverage of Proteus & Morganellea spp. | Can lead to Pseudomembranous colitis Causes haemolysis in G6PD deficiency Not recommended for children younger than 1 month | |
| 2. | Cephalexin ‘Keflex’ | 12.5mg/kg QID Max: 500 mg QID | 12.5 mg/kg Nocte Max: 25 0mg Nocte | Nausea and vomiting Cholestatic hepatitis Neurotoxicity Blood dyscrasia | E. coli P. mirabilis Klebsiella spp. | Prevalence of resistance varies by geography Risk of C. difficile, Candida and Enterococcus spp. infections |
| 3. | Amoxycillin and Clavulanic acid ‘Augmentin’ | 22.5 + 3.2 mg/kg BD Max: 875 + 125 mg BD | Not Recommended for prophylactic UTI treatment | Rash Transient deranged liver enzymes Nausea, vomiting, diarrhoea Cholestatic hepatitis Electrolyte disturbances Neurotoxicity Blood dyscrasia | Useful against b-lactamase strains of E. coli, Enterobacter spp. and Klebsiella spp. | Take with meals to enhance absorption Rashes are often associated concurrent infectious mononucleosis and/or leukaemia Risk of C. difficile, Candida and Enterococcus spp. infections |
| 4. | Norfloxacin ‘Noroxin’ | 10 mg/kg BD Max: 400 mg BD | Not Recommended for prophylactic UTI Treatment | Rash, pruritus Nausea, vomiting, diarrhoea Phototoxicity Hearing loss and diplopia Peripheral neuropathy Tendon rupture | Pseudomonas spp. Antibiotic resistant bacteria | Causes haemolysis in G6PD deficiency |
| 5. | Nitrofurantonin ‘Macrodantin’ | Not recommended for therapeutic UTI treatment | 1 mg/kg Nocte Max: 50 mg Nocte | Nausea, vomiting, diarrhoea Rash Vertigo Peripheral polyneuropathy Urine discolouration Hepatotoxicity is rare Pulmonary toxicity is rare | Gram negative and Gram positive coverage | Not recommended for children younger than 1 month Causes haemolysis in G6PD deficiency Antacids reduce potency of drug |
Treat children who have cystitis caused by P. aeruginosa with norfloxacin or ciprofloxacin as above; however, a longer treatment duration is often required

Algorithm for UTI management in children – Devised from the National Institute for Health and Care Excellence and Kidney Health Australia Guidelines
Urinary tract imaging (as per eTG)
The role of routine imaging to investigate for anatomical abnormalities after the first episode of urinary tract infection (UTI) in children is controversial.
The current trend is to limit imaging—particularly the use of dimercaptosuccinic acid (DMSA) scans, which are rarely indicated and result in a large radiation exposure.
Perform a renal ultrasound for children with:
- UTI due to atypical organisms (eg Pseudomonas species)
- concurrent bacteraemia
- an age less than 3 months
- kidney impairment
- significant electrolyte abnormality
- abdominal mass
- poor urinary stream
- failure to respond to appropriate antibiotics within 48 hours
- a first UTI if the child did not have a normal second or third trimester antenatal ultrasound that included the urinary tract
- recurrent symptomatic UTIs.
as per eTG – If the renal ultrasound is normal, further imaging is not required.
| KUB ultrasound First-line, non-invasive imaging | MCUG Contrast radiographic imaging | Nuclear scans DMSA and MAG3 Radioisotope nuclear imaging |
 |  |  |
| Uses | ||
|---|---|---|
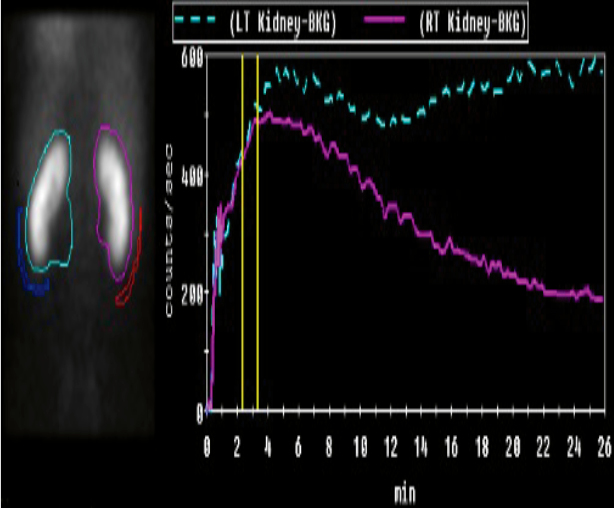
| Assess Fluid collections Bladder volume Kidney: size, shape, location Urinary tract: obstructions, dilatations | Confirm Posterior urethral valves Obstructive Uropathies Gold standard for VUR diagnosis | Confirm Suspicion of renal damage DMSA: Gold standard for renal scar detection MAG3: Faster, less radiationRenal excretion enables micturition study |
| Indications | ||
| Concurrent bacteraemia Atypical UTI organisms (Staphylococcus aureus, Pseudomonas) UTI <3 years old Non/inadequate response to 48hrs of IV antibiotics Abdominal mass Abnormal voiding Recurrent UTI First febrile UTI and no prompt follow up assured Renal impairment Significant electrolyte derangement No antenatal renal tract imaging in second to third trimester | Abnormal renal ultrasound (Hydronephrosis, Thick bladder wall, Renal scarring) Abnormal voiding post-febrile UTI Post-second febrile UTI Suspicion of VUR or posterior urethral valves | Clinical suspicion of renal injury Reduced renal function Suspicion of VUR Suspicion of obstructive uropathy on ultrasound in older toilet-trained children |
| Limitations | ||
| Does not asses function Operator dependent Cannot diagnose VUR | Radiation exposure ~1 mSv Invasive Unpleasant to perform post-infancy May require sedation Requires prophylactic antibiotics | Dynamic renal excretion study requires toilet training False positives if <3 months post-UTI, therefore can’t use in acute phase (0–4 weeks) May require sedation Cannot determine old versus new scarring |
| DMSA, dimercaptosuccinic acid -99mTc; KUB, kidneys, ureter and bladder; MAG3, mercapto-acetyl-triglycine-99mTc; MCUG, micturition urethrogram; mSv, millisievert; US, ultrasound; UTI, urinary tract infection; VUR, vesicoureteral reflux | ||
NICE Guidelines UK
- Children of all ages with atypical urinary tract infection perform ultrasound of urinary tract during the acute infection to identify structural abnormalitis
- Infants younger than 6 months + first time urinary tract infection that is responsive to treatment:
- do ultrasonography within 6 week of infection
- Children younger than <3 years with atypical and/or recurrent urinary tract infection:
- do a DMSA (dimercaptosuccinic acid) scan 4-6 months after the acute infection to detect renal parenchymal defects
- Do not do routine imaging to identify vesicoureteral reflux