Pre-excitation syndromes
Wolff-Parkinson-White (WPW) Syndrome
- WPW Syndrome refers to the presence of a
- congenital accessory pathway (AP) – Bundle of Kent and
- episodes of tachyarrhythmias.
- The term is often used interchangeablely with pre-excitation syndrome
- First described in 1930 by Louis Wolff, John Parkinson and Paul Dudley White
- Incidence is 0.1 – 3.0 per 1000

- Associated with a small risk of sudden cardiac death
- Pre-excitation
- refers to early activation of the ventricles due to impulses bypassing the AV node via an AP. Also known as bypass tracts, APs are abnormal conduction pathways formed during cardiac development and can exist in a variety of anatomical locations and in some patients there may be multiple pathways.
- In WPW, the AP is sometimes referred to as the Bundle of Kent, or atrioventricular bypass tract.

ECG features of WPW in sinus rhythm
- PR interval < 120ms
- Delta wave: slurring slow rise of initial portion of the QRS
- QRS prolongation > 110ms
- Discordant ST-segment and T-wave changes (i.e. in the opposite direction to the major component of the QRS complex)
- Pseudo-infarction pattern in up to 70% of patients — due to negatively deflected delta waves in inferior/anterior leads (“pseudo-Q waves”), or prominent R waves in V1-3 (mimicking posterior infarction)



Tachyarrhythmias associated with WPW syndrome
- Atrioventricular reentrant tachycardia (AVRT)
- FBI = Fast Broad Irregular tachycardia
Atrioventricular reentrant tachycardia (AVRT)
- is a supraventricular tachycardia that utilizes an accessory pathway between the atria and ventricles resulting in a circus movement.
- It is frequently, but not exclusively, associated with preexcitation syndrome (ie, the Wolff-Parkinson-White syndrome).
- The circuit involved in this reentrant arrhythmia includes the accessory bypass tract, AV node, and His Purkinje system, as well as the atria and ventricles.
- There is always 1:1 conduction of the impulse between the atria and ventricles since both structures, along with the AV node and accessory pathway, are a necessary part of the circuit.
- AVRT is often triggered by premature atrial beats or premature ventricular beats – retrograde activation of atria.
- Orthodromic AVRT accounts for >90% of AVRT and 20-30% of all sustained SVT.
- Based on direction of reentry circuit AVRT is divided into 2 groups:
- Orthodromic AVRT
- >90% of AVRT
- re-entrant impulse goes from the atrium to the ventricle through the AV node (normal ventricular activation) and then retrogradely activates atria through accessory pathway
- ECG:
- narrow complex tachycardia
- ventricular rate 150-250 bpm
- inverted P wave following a QRS complex – retrograde activation of the atrium
- short RP interval that is usually less than half of RR interval (< ½ RR)
- Antidromic AVRT
- the least common arrhythmia associated with WPW syndrome (3-8% of patients)
- Ventricles are activated through a very fast-conducting accessory pathway – anterograde conduction, atria are retrogradely activated over the AV node or another accessory pathway (30-60% of patients have multiple accessory pathways).
- ECG:
- wide QRS complex tachycardia
- ventricular rate 150-250 bpm
- Inverted P waves are often hidden in ST-T segment and therefore the RP interval is usually difficult to assess
- Orthodromic AVRT

WPW with AF – FBI = Fast Broad Irregular tachycardia
- this arrhythmia comes from a pre-excited atrial fibrillation that degenerates into FBI
- Paroxysmal AF has been found in 50% of patients with WPW
- Typically young patients with no structural disease of the heart
- atrial fibrillation with fast ventricular response over an accessory pathway
- potentially life-threatening arrhythmia – due to 1:1 conduction the ventricular rate may be very rapid (even >300bpm) and it can degenerate into ventricular fibrillation!
- ECG of atrial fibrillation in WPW:
- irregular wide complex tachycardia
- ventricular rate >200 bpm
- QRS complexes usually have variable morphology – APs bypassing the AV node can produce wide and bizarre looking complexes
- axis remains stable
- DO NOT give adenosine or amiodarone or B Blockers or Ca-Channel Blockers/verapamil (AV-nodal blockers) because can induce VFib
- Procainamide or cardioversion and then ablation

Management of AVRT
- Acute therapy
- Hemodynamically unstable patient – urgent synchronized cardioversion
- Hemodynamically stable patient
- Vagal manoeuvres
- Carotid sinus massage – Pressure is applied to one carotid sinus for 5 to 10 seconds. Steady pressure is recommended because it may be more reproducible. If the expected response is not obtained, the procedure is repeated on the other side after a one- to two-minute delay.
- Valsalva manoeuvres – patient is instructed to exhale forcefully against a closed glottis (against closed mouth and compressed nose) for 10 – 15s and then release.
- Modified Valsalva manoeuvre – patient does classical Valsalva manoeuvre followed by 15 seconds of passive leg raise at 45 degree angle – this may be more successful in restoring sinus rhythm.
- Vagal manoeuvres
- If vagal manoeuvres are ineffective:
For orthodromic AVRT:
- Adenosine
- use with caution! – potential induction of atrial fibrillation with fast ventricular conduction or ventricular fibrillation
- electrical cardioversion should always be available when administering adenosine
- 6 mg i.v. as a rapid bolus with saline flush
- second dose – 12 mg i.v., safe within 1 min of the last dose
- maximum dose = 18 mg
- If Adenosine is ineffective > pharmacological therapy directed at AV node:
- Beta blockers – i.v. esmolol, i. v. metoprolol
- Calcium channel blockers (verapamil/diltiazem i.v.)
- If this ineffective > Synchronized cardioversion
For antidromic AVRT:
- If vagal manoeuvres are ineffective:
- Pharmacological therapy directed at fast-conducting AP (accessory pathway):
- i.v. ibutilide or procainamide
- i.v. propafenone or flecainide
- Synchronized cardioversion
- Pharmacological therapy directed at fast-conducting AP (accessory pathway):
- Chronic therapy
- The treatment of choice for patients with symptomatic and recurrent AVRT is catheter ablation of accessory pathway
- Propafenone or flecainide may be considered in patients with AVRT and without ischaemic or structural heart disease, if ablation is not desirable or feasible
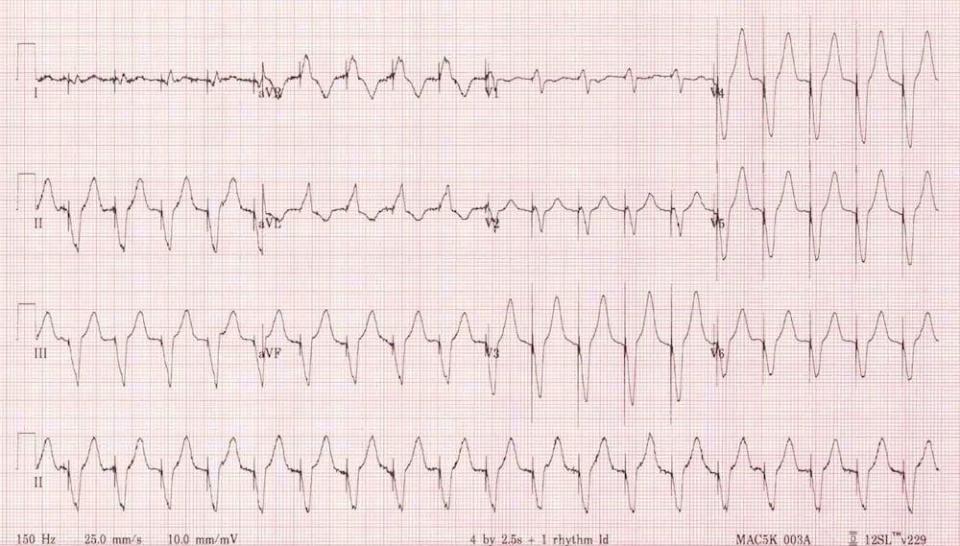
ECGS:

Main Abnormalities:
Irregularly irregular broad complex tachycardia
Extremely rapid ventricular rates — up to 300 bpm in places (RR intervals as short as 200ms or 1 large square)
Beat-to-beat variability in the QRS morphology, with subtle variation in QRS width
Explanation of ECG Findings:
Irregularly irregular rhythm is consistent with atrial fibrillation
There is a left bundle branch block morphology to the QRS complexes
However, the ventricular rate is far too rapid for this to be simply AF with LBBB
The rates of 250-300 bpm and the variability in QRS complex morphology indicate the existence of an accessory pathway between the atria and ventricles
Diagnosis: These findings indicate atrial fibrillation in the context of Wolff-Parkinson-White syndrome
EXAMPLES
Broad complex irregular tachycardia at very rapid rates? -> Suspect AF with WPW!
These patients can rapidly become haemodynamically unstable
The options for chemical cardioversion are very limited, favouring DC cardioversion
We would recommend immediate DC cardioversion in this patient. Our approach would be:
Fluid load with 0.5 – 1L crystalloid bolus
Add in a push-dose vasopressor to elevate the BP (e.g. Metaraminol 0.5 – 1mg IV)
Sedate with something that has minimal effects on BP (e.g. fentanyl or ketamine in cautious doses)
Shock at 200J biphasic. Consider using an AP pad position for maximal 1st shock success

Clue: patient 5 years old
Antidromic atrioventricular re-entry tachycardia (AVRT) due to Wolff-Parkinson-White syndrome
This is the one rhythm that may be impossible to distinguish from VT!
In this case the main clue is the history — more than 95% of broad complex tachycardias in children are SVT with aberrancy
There are obvious pacing spikes before each QRS complex
Ventricular paced rhythms have features in common with other ventricular rhythms — in this case the ECG demonstrates negative concordance in V1-6, initial R wave > 40ms in V1, RS interval > 70 ms in V1, QS complex in V6
Remember that the pacing spikes may not always be as obvious as this!