Red Rashes on Face
Background
- Prevalence: Red facial rashes are a common presentation in general practice in Australia.
- Impact: Significantly affects quality of life due to the cosmetic sensitivity of the face.
- Importance: Accurate diagnosis is essential for appropriate treatment.
Assessment and Diagnosis
- History and Examination: A thorough history and physical examination are often sufficient to diagnose common facial rashes.
- Differential Diagnosis: Wide range, categorized by age, morphology, and distribution. Key factors include symptomology, age of onset, rash morphology, and clinical clues.
Common Causes and Clinical Features
- Atopic Dermatitis (Eczema)
- Morphology: Erythema, scale, excoriations, xerosis, lichenification; honey-colored crusts if infected.
- Distribution: Face, neck, scalp, eyelids (Dennie–Morgan folds), lips (licker’s eczema).
- Clinical Clues: History of atopy (asthma, allergic rhinitis, eczema), keratosis pilaris on upper arms/thighs, significant itch, predilection for face/neck suggesting aeroallergens.
- Diagnostic Tests: Clinical diagnosis, bacterial culture if infected, allergen-specific IgE testing, skin biopsy if unclear.
- Irritant Contact Dermatitis
- Morphology: Xerosis, erythema, scale; worse in skin creases.
- Distribution: Corners of mouth, ala creases; sparing of eyelids, ears, frontal hairline.
- Clinical Clues: Timeline with new products, over-cleansing, more common in atopic dermatitis patients.
- Diagnostic Tests: Clinical diagnosis, cessation of irritant products.
- Psoriasis
- Morphology: Well-defined, scaly, salmon-pink plaques.
- Distribution: Ears, scalp (especially frontal hairline, occipital scalp), extensors, umbilicus, natal cleft.
- Clinical Clues: Personal or family history of psoriasis, might have seborrhoeic dermatitis.
- Diagnostic Tests: Clinical diagnosis, skin biopsy if unclear.
- Seborrhoeic Dermatitis
- Morphology: Ill-defined erythema, greasy scale.
- Distribution: Scalp, forehead, eyebrows, nasolabial folds, conchal bowl, post-auricular.
- Clinical Clues: History of dandruff, winter flares, relatively asymptomatic.
- Diagnostic Tests: Clinical diagnosis, skin biopsy if unclear.
- Actinic Keratoses
- Morphology: Ill-defined erythema and scale, hyperkeratotic papules or nodules.
- Distribution: Photo-exposed sites (nose, cheeks, temples, ear helices); scalp if bald.
- Clinical Clues: History of chronic sun exposure, asymptomatic.
- Diagnostic Tests: Skin biopsy, especially for hyperkeratotic or indurated lesions.
- Acne
- Morphology: Polymorphic erythematous papules, pustules, nodules; comedones, postinflammatory pigmentation, scars.
- Distribution: Face, back, chest.
- Clinical Clues: Onset around puberty, family history of acne, possible steroid use.
- Diagnostic Tests: Clinical diagnosis.
- Rosacea
- Morphology: Erythematous papules, pustules; telangiectasia, erythema.
- Distribution: Dorsum of nose, cheeks, chin, forehead.
- Clinical Clues: Flushing with heat, alcohol, spicy food; family history of rosacea.
- Diagnostic Tests: Clinical diagnosis.
- Malassezia Folliculitis
- Morphology: Monomorphic erythematous papules, pustules based around hair follicles.
- Distribution: Forehead, chin, lateral cheeks, central face spared.
- Clinical Clues: Oily skin, flares with heat, sweat, occlusion.
- Diagnostic Tests: Clinical diagnosis, yellow–orange fluorescence on Woods lamp, KOH test of skin scrapings.
- Pseudofolliculitis Barbae
- Morphology: Erythematous papules, sterile pustules around hair follicles.
- Distribution: Beard area (cheeks, upper lip, chin, neck).
- Clinical Clues: Hair removal practices, curly hair, common in men of African ancestry.
- Diagnostic Tests: Clinical diagnosis, bacterial culture, fungal scrapings.
- Sunburn
- Morphology: Erythema, edema, blistering in severe cases; peeling and flaking during resolution.
- Distribution: Photo-exposed sites (face, trunk, limbs).
- Clinical Clues: Associated with sun exposure, sharp cut-off from clothing.
- Diagnostic Tests: Clinical diagnosis.
- Periorificial Dermatitis/Steroid-Induced Rosacea
- Morphology: Numerous papules, pustules; erythematous, oedematous, scaly.
- Distribution: Around orifices (mouth, nose, eyes), sparing vermillion border.
- Clinical Clues: Steroid exposure, paradoxical flare with cessation.
- Diagnostic Tests: Clinical diagnosis.
- Tinea Faciei
- Morphology: Annular eruption, leading edge, central clearing, peripheral scale.
- Distribution: Face, neck, scalp.
- Clinical Clues: Paradoxical worsening with steroids, recent barber visit, pets with scaly patches.
- Diagnostic Tests: Skin scrapings for fungal microscopy and culture, skin biopsy if unclear.
- Allergic Contact Dermatitis
- Morphology: Oedema, erythema, vesicles or bullae.
- Distribution: Eyelids, lips, neck, other exposed areas.
- Clinical Clues: Triggered by products/chemicals, itch.
- Diagnostic Tests: Clinical diagnosis, allergy patch testing, skin biopsy if unclear.
- Shingles
- Morphology: Erythematous papules, macules; vesicles, crusting.
- Distribution: Dermatomal, unilateral.
- Clinical Clues: Burning, pain or tingling before rash, systemic symptoms.
- Diagnostic Tests: VZV swab for PCR.
- Cutaneous Lupus
- Morphology: Smooth, erythematous plaques (acute); scaly hyperpigmented plaques with follicular plugging (discoid).
- Distribution: Butterfly distribution (cheeks, nose), other photo-exposed areas.
- Clinical Clues: Systemic lupus symptoms.
- Diagnostic Tests: Skin biopsy, ANA, ENA, dsDNA, complement, urine microscopy.
- Dermatomyositis
- Morphology: Pink to violaceous erythema of eyelids, scaling on scalp.
- Distribution: Eyelids, forehead, scalp.
- Clinical Clues: Muscle weakness, photosensitivity, other signs of dermatomyositis.
- Diagnostic Tests: Skin biopsy, CK, myositis-specific antibodies, malignancy screening.
- Systemic Conditions (e.g., pulmonary hypertension, liver failure, SVC obstruction, carcinoid syndrome)
- Morphology: Plethora, fixed erythema, edema, flushing.
- Distribution: Variable, can involve cheeks, forehead, periorbital region, neck.
- Clinical Clues: Known comorbidities, systemic symptoms (dyspnea, weight loss, jaundice).
- Diagnostic Tests: ECG, liver function tests, full blood count, renal function test, chest X-ray, echocardiogram, 24-hour urinary 5-HIAA.
| Causes of red rashes on the face | ||||
|---|---|---|---|---|
| Diagnosis | Morphology | Distribution | Clinical clues | Diagnostic tests |
| Atopic dermatitis (eczema) | Erythema, scale, excoriations, xerosisLichenification Ill-defined plaques Honey-coloured crusts if secondarily infected | Anywhere on face, neck, scalp Variants: – NeckLips (eg licker’s eczema) – Eyelids (eg Dennie–Morgan folds) – Might have eczema elsewhere (eg flexures, nipples, palmoplantar [dyshidrotic eczema]) | History of atopy (eg asthma, allergic rhinitis, eczema [including in family members]) Keratosis pilaris on upper arms/thighs Lichenification suggestive of chronicity Itch can be significant Predominance of face/neck eczema might suggest aeroallergens (eg dust mites, pollen, grasses, animal dander) | Clinical diagnosis Bacterial MCS if secondarily infected Allergen-specific IgE testing for common aeroallergens if indicated Skin biopsy: histopathology if diagnosis unclear |
| Irritant contact dermatitis | Xerosis Erythema and scale might be present | Worse in skin creases (eg corners of mouth, ala creases) Sparing of eyelids, ears, frontal hairline or neck if irritant not in contact with those areas | Timeline with use of one or more new products Over-cleansing of face Might or might not be itchy Patients with atopic dermatitis more prone to developing irritant contact dermatitis Might have single exposure to strong irritant or chronic exposure to weak irritants | Clinical diagnosis Cessation of new or unnecessary products and gentle skin care (eg bland unscented moisturiser, sunscreen) |
| Psoriasis | Well-defined, scaly, salmon-pink plaques Scale can be significant especially in scalp | Favours ears and scalp (especially frontal hairline and occipital scalp) Might have psoriasis elsewhere (eg extensors, umbilicus, natal cleft, palmoplantar) | Mostly asymptomatic but can be itchy Concurrent seborrhoeic dermatitis (sebopsoriasis) Personal or family history of psoriasis | Clinical diagnosis Skin biopsy: histopathology if diagnosis unclear |
| Seborrhoeic dermatitis | Ill-defined erythema, greasy scale | Favours seborrhoeic areas: scalp, forehead, eyebrows, nasolabial fold, conchal bowl, post-auricular | History of dandruff or flaking scalp Other sites might be involved including chest, axillae Can be itchy if inflamed, otherwise relatively asymptomatic Winter flares with improvement in summer | Clinical diagnosis Skin biopsy: histopathology if diagnosis unclear |
| Actinic keratoses | Ill-defined erythema and scale Might be discrete or confluent to involve large areas Hyperkeratotic papules or nodules in some areas | Photo-exposed sites (eg nose, cheeks, temples, ear helices); scalp involvement if bald or thin hair Might have actinic keratoses elsewhere (eg dorsal hands, forearms, lower legs Sparing of photoprotected sites | Asymptomatic Gradual onset over time History of chronic sun exposure/limited photoprotection No history or other features of primary dermatosis | Skin biopsy: histopathology (particularly for hyperkeratotic, tender or indurated lesions to exclude invasive SCC) |
| Acne | Polymorphic erythematous papules, pustules and nodules Cysts might be present in severe cases Closed or open comedones Post inflammatory pigmentation Excoriations (if picking) Acne scars (eg box car, rolling, atrophic, ice pick scars) | Favours face, back and chest | Family history of acne Papules, pustules and nodules are in different stages of evolution Teens: onset around puberty Adults: persistence since teens or onset early 20s. In women, might flare with menses Might be associated with testosterone or anabolic steroid usage | Clinical diagnosis |
| Rosacea | Monomorphic erythematous papules and pustules (papulopustular subtype) Absence of comedones (unless there is co-existing acne) Telangiectasia and erythema (in erythematotelangiectatic subtype) | Favours dorsum of nose, cheeks, chin, forehead | Favours fair-skinned patients Might be associated with flushing History of sensitive skin to various products Flares with sun exposure Family history of rosacea | Clinical diagnosis |
| Malassezia folliculitis | Monomorphic erythematous papules and pustules based around hair follicles Absence of comedones | Favours forehead, chin, lateral cheeksCentral face usually spared Chest and back might be involved | Might have other forms of cutaneous Malassezia spp. overgrowth (eg seborrhoeic dermatitis, pityriasis versicolour)Oily skin Flares with heat, sweat, occlusion or in hot, humid conditions Might be itchy | Clinical diagnosis Yellow–orange fluorescence on Woods lamp Skin scrapings of a pustule, KOH test (culture not routinely performed because isolation and culture of Malassezia spp. is difficult) |
| Pseudofolliculitis barbae | Erythematous papules and sterile pustules based around hair follicles Associated ingrown hairs Postinflammatory pigmentation | ‘Beard’ area of the face (ie cheeks, upper lip, chin, neck) | Flares with hair removal (eg shaving, waxing, plucking)Favours patients with curly hair Most common in men with African ancestry Might be itchy | Clinical diagnosis Bacterial MCS to exclude bacterial folliculitis Fungal skin scrapings to exclude tinea barbae |
| Sunburn | Acute phase: erythema and oedema; blistering in severe cases Resolution phase: peeling and flaking of affected skin | Photo-exposed sites (eg face, trunk, limbs)Sharp cut-off and sparing of areas covered by clothing Associated ephelides or lentigines (if chronic) in sun-exposed sites | Associated with total duration of sun exposure and UV index Favours patients with lighter skin phototype Might be more likely to occur if taking photosensitising medications | Clinical diagnosis |
| Periorificial dermatitis/steroid-induced rosacea | Classically numerous papules and pustules; might be more confluent than rosacea Absence of comedones Might be erythematous, oedematous and scaly in some cases | Clustered around orifices (eg skin inferior to nostrils, chin, lateral cheeks/temples around eyelids)Sparing vermillion border of lip | Might be associated with steroid exposure (eg topical mid- to high-potency steroids). Other triggers include intranasal/inhaled or oral steroids Paradoxical flare with cessation of steroid Associated stinging or burning sensation | Clinical diagnosis |
| Tinea faciei | Annular eruption with a leading edge, central clearing and peripheral scale Might become non-scaly/non-specific if treatment modified with topical steroids (tinea incognito) | Anywhere on face, neck, scalp | Paradoxical worsening with use of topical steroids Asymmetrical History of recent visit to barber Pets with scaly patches of hair loss (eg cats, dogs, guinea pigs)Might have associated onychomycosis | Skin scrapings for fungal microscopy and culture Skin biopsy (if required): histopathology |
| Allergic contact dermatitis | Acute phase: oedema, erythema, vesicles or bullae Chronic phase: mimics atopic dermatitis (erythema, scale, excoriations, lichenification) | Common sites: eyelids, lips/perioral skin, neck Other sites also exposed to allergen might be affected | Can occur to products/chemicals that have previously been tolerated for many months or years, not just newly introduced products Associated itch In acute phase might be triggered 24–48 h following exposure to allergen Ongoing exposure can lead to chronic phase | Clinical diagnosis Referral for allergy skin patch testing Skin biopsy: histopathology if diagnosis unclear |
| Shingles | Prevesicular phase: crops of erythematous papules and macules Vesicular phase: pustules, vesicles followed by crusting | Favours dermatomal distribution or is unilateral Might be multidermatomal or disseminated, especially in immunosuppressed patients | Associated burning, pain or tingling sensation precedes skin manifestations Might be associated with systemic symptoms (eg malaise)Red flags: ocular involvement, facial weakness, ear canal involvement | VZV swab for PCR |
| Cutaneous lupus | ACLE: smooth, erythematous, oedematous plaques DLE: coin-shaped, scaly hyperpigmented plaques, follicular plugging. Might have scarring Note: subacute cutaneous lupus erythematosus might less commonly present on the face as annular scaly plaques | ACLE: ‘Butterfly’ distribution, namely bilateral cheeks and across the dorsum of the nose, sparing nasolabial folds. Can affect other photo-exposed sites DLE: face, scalp, conchal bowl and ears. In diffuse form, might occur on trunk | Might have associated systemic symptoms of lupus (eg synovitis, chest pain, shortness of breath) | Skin biopsy: histopathology, direct immunofluorescence Blood tests: ANA, ENA, dsDNA, complement Urine microscopy: proteinuria, dysmorphic red blood cells, red cell casts |
| Dermatomyositis | Pink to violaceous erythema of eyelids; might have associated oedema (heliotrope rash) Erythema, scale and diffuse alopecia affecting the scalp | Eyelids, forehead, scalp Might have other clinical signs of dermatomyositis (eg shawl sign, V-neck sign, Holster sign, Gottron’s papules, Gottron’s sign, nail fold changes) | Might have associated muscle weakness (except in amyopathic forms)Associated photosensitivity | Skin biopsy: histopathology Special blood tests: CK, myositis-specific antibodies Consider malignancy screen |
| Facial erythema secondary to a non-dermatological systemic process (eg pulmonary hypertension, liver failure, SVC obstruction, carcinoid syndrome) | Plethora, fixed erythema, oedema, facial flushing Absence of more specific skin changes such as pustules, papules, scale, vesicles or erosions | Variable distribution Might present as facial flushing, fixed erythema and telangiectasia involving the cheeks, forehead, periorbital region and/or neck Might also involve other body sites (eg palmar erythema, spider naevi on chest) | Known respiratory, gastrointestinal or cardiovascular comorbidities Systemic symptoms such as dyspnoea, hoarse voice, chest pain, weight loss, fatigue, peripheral oedema, diarrhoea and/or jaundice Abnormal cardiorespiratory and/or gastrointestinal examination | Depending on suspected cause: Electrocardiogram Bloods: liver function test, full blood count, renal function test Chest X-rayEchocardiogram24-h urinary 5-HIAA for suspected carcinoid syndrome |
| 5-HIAA, 5-hydroxyindoleacetic acid; ACLE, acute cutaneous lupus erythematosus; ANA, antinuclear antibodies; CK, creatine kinase; DLE, discoid lupus erythematosus; dsDNA, double-stranded DNA; ENA, extractable nuclear antigen antibodies; IgE, immunoglobulin E; KOH, potassium hydroxide; MCS, microscopy, culture, sensitivity; PCR, polymerase chain reaction; SCC, squamous cell carcinoma; SVC, superior vena cava; UV, ultraviolet; VZV, varicella zoster virus. | ||||
| Causes of red rashes on the face categorised by typical age of onset | ||
| Age 20–40 years | Age 40–60 years | Age >60 years |
| Common: Acne vulgaris Atopic dermatitis Rosacea Seborrhoeic dermatitis Periorificial dermatitis/steroid-induced rosacea Irritant contact dermatitis Sunburn Less common: Psoriasis Allergic contact dermatitis Malassezia folliculitis Pseudofolliculitis barbae Tinea faciei Cutaneous lupus erythematosus | Seborrhoeic dermatitis Rosacea Irritant contact dermatitis Allergic contact dermatitis Actinic keratosis Shingles Cutaneous lupus erythematosus Dermatomyositis | Seborrhoeic dermatitis Atopic dermatitis Psoriasis Actinic keratosis Shingles Cutaneous lupus erythematosus Dermatomyositis |
Approach to Diagnosis
- History of Presenting Issue:
- Clarify onset, symptomology, effects on quality of life.
- Assess age of onset and pattern of involvement.
- Evaluate distribution for possible causes.
- Examination:
- Characterize distribution and predominant morphology.
- Classify rashes under scaly, papulopustular, and mixed morphology.
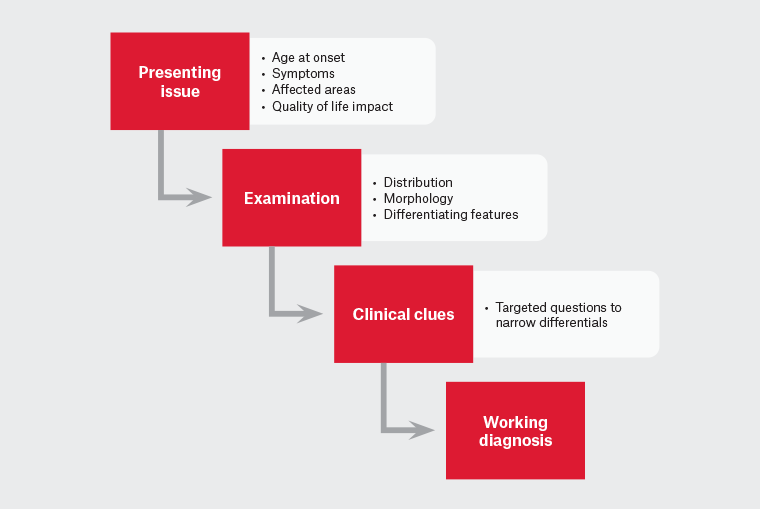
Figure 1. Suggested approach to red rashes on the face.
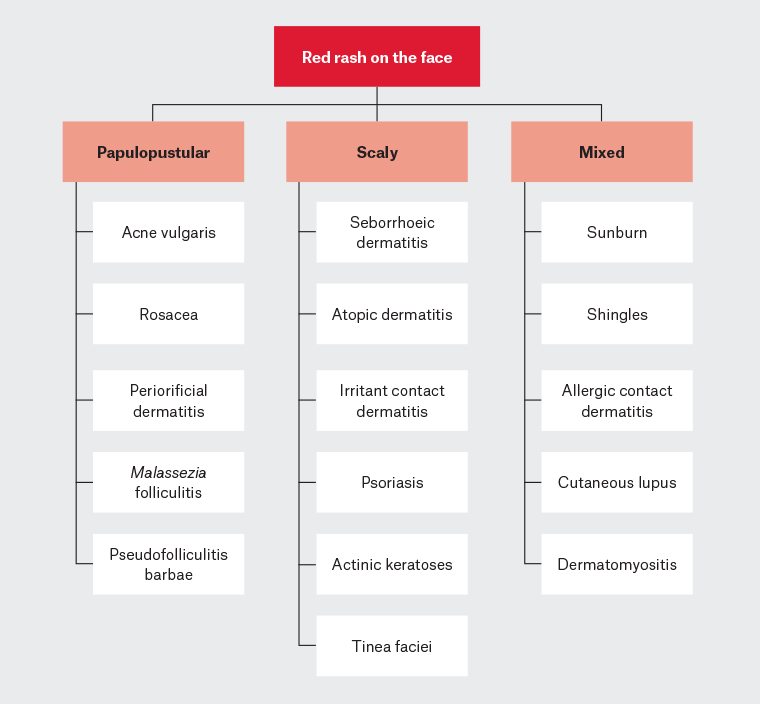
Figure 2. Causes of red facial rashes categorised by predominant morphology.
Clinical Clues:
- Use targeted questions to narrow differential diagnosis based on history and examination findings.
Investigations:
- Swabs for bacterial culture.
- Skin scrapings for fungal microscopy and culture.
- Swab for VZV PCR.
- Skin biopsy for unclear diagnoses or non-responsive cases.
Conclusion
- Accurate diagnosis of red facial rashes can often be achieved through a thorough clinical assessment, supported by appropriate investigations when necessary.