- Associated with Inflammatory Bowel Disease
- Greater association with Crohn’s Disease
- No synovial destruction
- Course
- Does not resolve after proctocolectomy
- Often subsides in 6-8 weeks after onset
- Often recurrs and may become chronic in 10% of cases
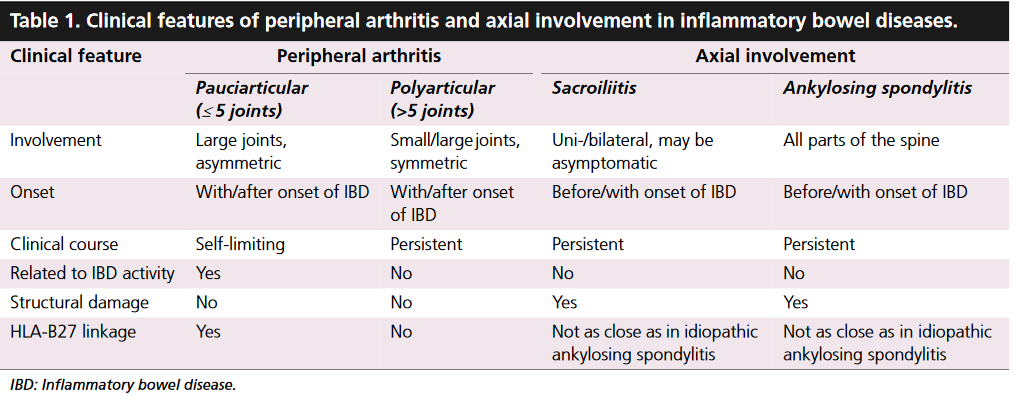
- Symptoms
- Asymmetric joint involvement
- Migratory Arthritis or Monoarticular Arthritis
- Lower extremity more often involved
- Joints affected
- Hip
- Ankle
- Low Back Pain with morning stiffness
- Associated Spine conditions
- Ankylosing Spondylitis
- Sacroiliitis
- Axial Arthritis
- Extra-articular changes
- Bilateral Uveitis
- Skin changes
- Erythema Nodosum
- Pyroderma gangrenosum
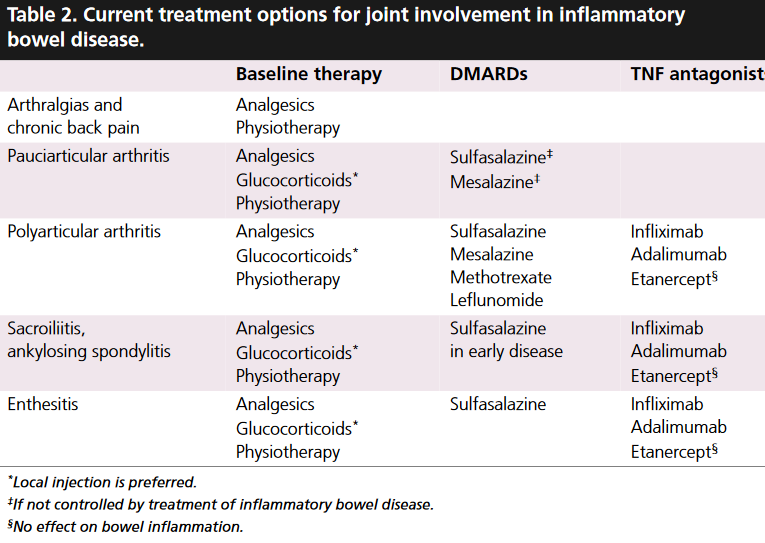
- Management
- Avoid NSAIDs if possible
- Sulfasalazine
- Methotrexate
- Azathioprine
- Etanercept (TNF-a inhibitor)
Related